Juan Ding, OD, PhD
I look at eyes all day, and have to admit that I care less about anything else. But this case was a big help from another specialty which not only nailed the diagnosis but also saved a lot of $$$ and time on the expensive and lengthy tests that we so often have in the health care.
Case: visiting the eye doctor
A man in his mid 50s, Edward, we will call him, came into the office complaining about new floaters in the left eye for 1 week. This is a very common complaint, which I hear about almost daily.
If you read my previous posts, you would know that the most common cause of floaters are vitreous degeneration or detachment (link and also here) and the biggest worry would be that there was a retinal tear or detachment in the process (Refer to Figure 1 below for these structures: vitreous and retina).
He saw no flashes, and there was no injury to the eyes or the head. He had no pain and no visual changes.
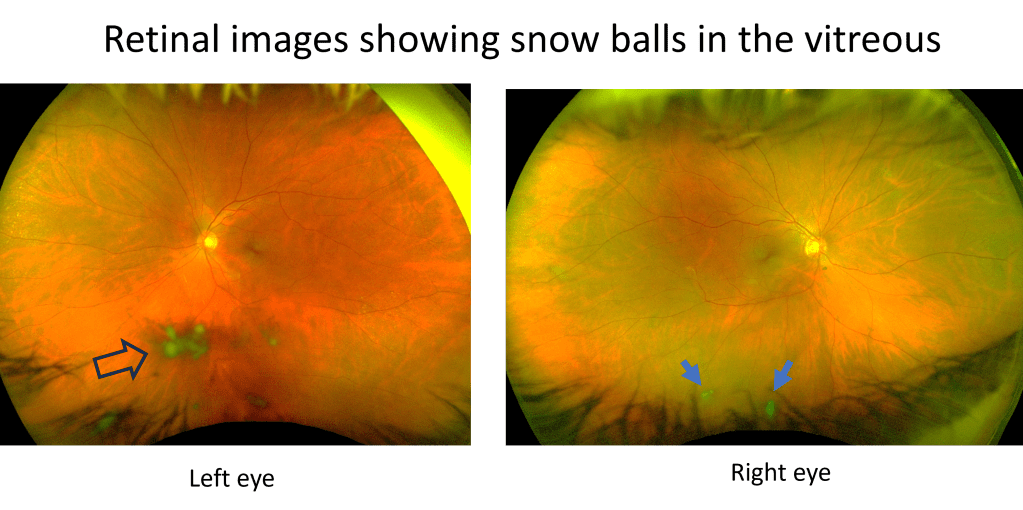
The exam showed normal vision, normal eye pressure, and interestingly no vitreous detachment. However, there were some cells in the vitreous in the left eye (again refer to Figure 1 to see where the vitreous is in the eye). The retina appeared normal without any tear or detachment. A closer looked showed that there were even cells in anterior chamber, the front chamber of the eye (in contrast, the vitreous is the back chamber of the eye).

So this was a form of uveitis, which is less common, but also can cause floaters, which I talked about in a previous case also (link).
Uveitis is the inflammation of the colored layer of the eye, called uvea (Figure 1). Injuries can cause this inflammation, but so can infections, autoimmune diseases, cancer and sometimes no reason that we can find.
The question is, what is causing the uveitis?
More about this patient
I asked him if there was anything else going on besides the eyes?
He said, ‘I have had a skin rash on my back before the floaters showed up. My dermatologist gave me a fungal cream but it’s not working and I am going back to see him next week.’
Otherwise he was in his usual health with no complaints.
Looking at his other office visits, I could see that he fought two cancers, once 10 years ago and once 5 years ago. Fortunately both were found in stage 1 and adequately treated.
He was HIV positive, but had normal CD4 values and was taking his anti-virals consistently. He was also being tested regularly on chlamydia and syphilis and negative in these in the last labs 4 months ago.
Based on this history, cancer is a concern. But HIV related etiologies are also possible. These both can cause uveitis. Further, inflammatory causes (non-cancer, non-infectious) are also possible.
Cause of uveitis revealed by skin test
I promptly referred him to our uveitis specialist, who will run a battery of tests and imaging to figure out what is the cause.
However, it was his dermatologist that nailed the diagnosis and sent him for the definitive treatment.
Since the rash did not improve with medical treatment, his dermatologist performed a skin biopsy, which showed a very small bug (called spirochetes), the causative agent for the rash, and also the uveitis in the eye. These spirochetes are the microorganisms that cause syphilis, a sexually-transmitted disease that is sometimes found to be more prevalent in those with positive HIV.
In this case, a simple skin biopsy saved him the trouble of a battery of tests and imaging procedures, which was the silver lining of his unfortunate symptoms. The treatment, IV penicillin, is usually quite effective.
Additional thoughts
In the end, this outcome might be the best it can be. Cancer in the eye, such as lymphoma, would be much more difficult to get rid of, not to mention possibility of death.
As an eye doctor, the most important thing is not to mis-diagnose this special form of uveitis as the good old vitreous detachment, even though vitreous degeneration or detachment is the horse, and uveitis is the zebra.
And syphilis, a great mimicker of all forms of uveitis, should always be tested, especially if the patient is at risk.
So if you have new floaters, please reach out to an eye doctor, because your retina may be at risk and it could be something else.
Learn more about uveitis from this reference below.
Reference
[1] Uveitis, National Eye Institute, https://www.nei.nih.gov/learn-about-eye-health/eye-conditions-and-diseases/uveitis