A guide to LASIK, PRK and SMILE
Refractive surgery to correct myopia and hyperopia has been around for many years, with technology evolving from micro blade to all laser today. More and more patients have undergone refractive surgery and said goodbye to their glasses. Many people wish they had done it sooner, but more people are still debating, should I have it done? If so, with all these technologies, which one to choose?
What is the difference between LASIK, PRK and SMILE?
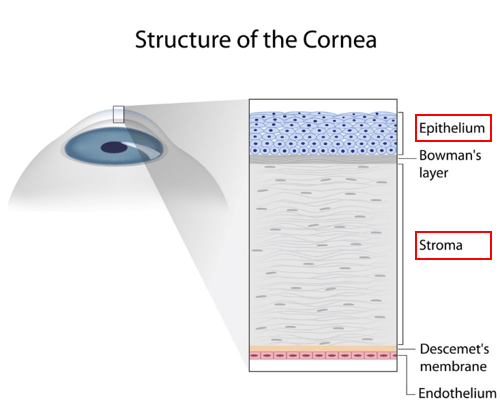
There are several corneal refractive surgeries, the most mature and commonly used of which is LASIK (laser-assisted in situ keratomileusis). FDA approved LASIK to be used in myopia < -11.00 D with astigmatism < 2.00 D; or in hyperopia < +3.00 D with astigmatism < 2.00 D; in patients 18 or older. LASIK operates on cornea, a thin transparent tissue shaped like a convex lens covering the front of the eye. The cornea is composed of five layers, the most front thin layer being the epithelium, followed by a much thicker stromal layer (Figure 1). These two layers are critical for understanding how corneal refractive surgery works.
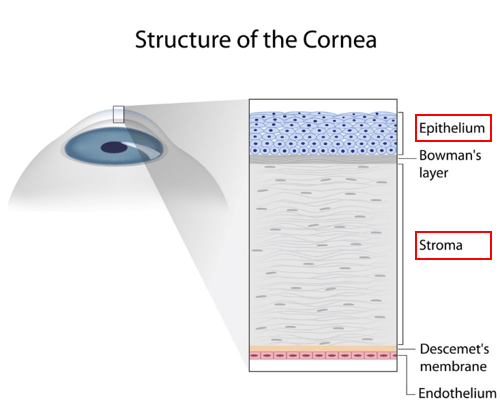
Figure 1. Layers of cornea showing the epithelium and stroma. (Image source: http://discoveryeye.org/treatment-corneal-scratches-and-abrasions/)
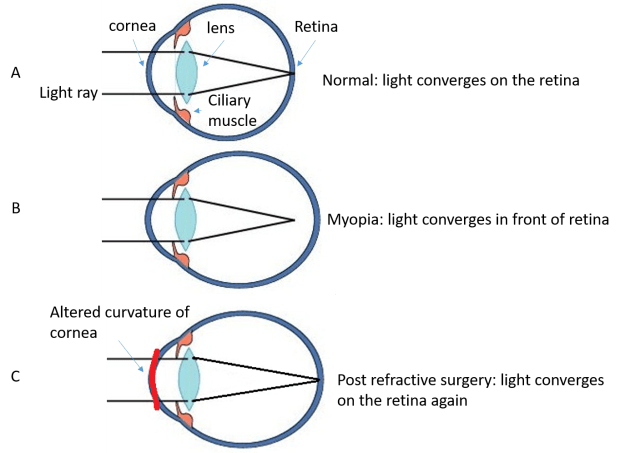
Myopia is caused by elongated eye axis resulting in distant light converge in front of the retina (myopia in Figure 2B compared to normal in Figure 2A). You can read more on myopia in my other post [link here]. No surgery can shorten the axis of the eye, but it is surgically possible to reduce the refractive power of the cornea, so that light converges less and reaches the retina again (Figure 2C). In refractive surgery for myopia, a specific amount and shape of the corneal stromal tissue is removed to make the cornea flatter. For hyperopia, opposite strategy is used, the corneal tissue is reconstructed to be steeper.
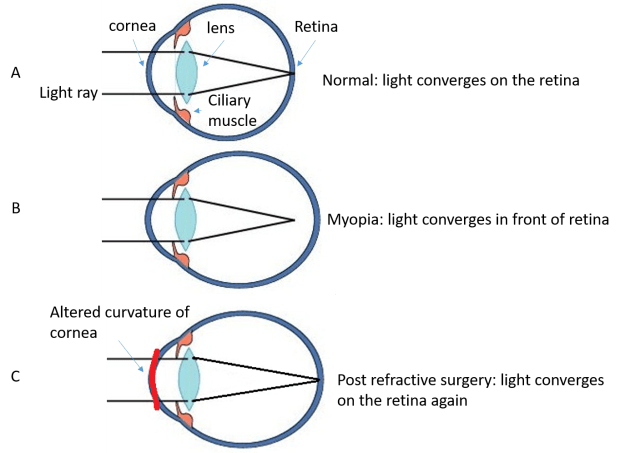
Figure 2:How corneal refractive surgery corrects myopia.
LASIK
The procedure of LASIK is shown in Figure 3. First, a flap is made on the surface (the epithelium and a very thin layer of the stroma) of the cornea (Figure 3A), then a specific amount and shape of the stromal tissue is ablated by laser (Figure 3B), followed by repositioning of the flap (Figure 3C and D). As a result, cornea becomes flatter and myopia is corrected. LASIK technology has become very sophisticated, with the option of wave-front guided customization to minimize higher order aberration, iris registration to track eye movement, and of course, a femtosecond laser used to create the flap. Prior to 2000, the flap was created using a micro blade surgically. Femtosecond laser is a laser that has very high frequency and high energy, which enables quick and accurate incision of tissue. The modern LASIK uses femtosecond laser to create flap, not only being more accurate, but also reducing complications related to the flap compared to micro blade. Still, the flap may dislocate after the surgery, therefore patient is advised not to rub their eyes or do heavy exercises for a week, scuba dive for a month and do kickboxing or jumping out of an airplane for 3 months after LASIK.

Figure 3:Illustration of LASIK procedure. (Image source: http://www.wfeye.net/type/jzjs/LASIK/)
I remember the first time watching a video on LASIK done on a real patient. I was shocked. It was a huge flap to take off, and it felt painful. Of course it is a painless procedure, it just looks painful. I had mine done 13 years ago in Beijing. Had I watched such a video then, I might not have the gut to go under the table. As research has shown, fear is the number 1 reason to hold back patients in their decision to pursue refractive surgery.
PRK
If a flap on the cornea is not desired due to, for example, being a soldier, an alternative laser surgery called PRK (photorefractive keratectomy) can be used. In this method, the entire corneal epithelium is removed, then the right amount of corneal stromal tissue is ablated similar to that in LASIK. Because no flap is made, complications related to the flap as in LASIK are not an issue. In addition, because the flap contains some stromal tissue, LASIK requires more starting corneal thickness than PRK; thus PRK can be used in certain patients whose cornea thickness is not enough for LASIK. However, the disadvantages of PRK compared to LASIK include more pain and discomfort post operation, as the corneal epithelium which is removed contains large amount of nerves; also, because the epithelium is removed entirely, it takes significantly longer to heal and recover, and extra care is needed to prevent infection. In general, people feel ‘wow, the world is clear’ right after or the next day after LASIK, whereas it will take a week for PRK patients to see the world clearly. You also need to have more frequent follow up visits for PRK vs LASIK. Therefore PRK is usually reserved for those who cannot have LASIK done for various reasons.
SMILE
Now a new technology has come out, Small Incision Lenticule Extraction (SMILE). In this procedure, everything is done by femtosecond laser, and a flap is no longer used. SMILE has been popular in Europe and Asia for a few years now, and has only been approved by FDA recently (September 2016). FDA approved SMILE to be used for myopia of -1.00 to -8.00 with astigmatism of 0.50 D or less, in patients aged 22 and older. In this procedure, a femtosecond laser makes cuts within the cornea, creating a disc-shaped piece of tissue that is removed through a small incision in the surface of the cornea. The small incision is only 2-4 mm compared to a flap diameter of 8-9 mm (or 20 mm circumference). Figure 4 shows the difference in incision on the cornea by SMILE vs LASIK. Because of less damage to the cornea and corneal nerves, it is found that people have better corneal sensitivity and less subjective feeling of irritation and discomfort after SMILE compared to LASIK [1, 2].

Figure 4:Difference in incision size between SMILE and LASIK (image adapted from: http://www.euroeyes.cn/relex-smile/)
Are they all the same?
In terms of efficacy, all 3 technologies are similar. The difference lies in post op recovery (quick in LASIK and SMILE, slower in PRK), flap related complications (only in LASIK), and dry eye symptoms (least in SMILE). In addition, price is a factor. The latest LASIK technology containing femtosecond laser creating flap, wave-front guided customization, iris registration etc costs about $2,000 per eye (this is only a rough estimate, prices vary in different clinics), with similar price in PRK; while SMILE is still new in the US, the price is about 30% higher than LASIK in China and Singapore.
Should I do it or not?
Refractive surgery is an elective surgery, that is, it is considered cosmetic and not covered by insurance. To do it or not depends on personal needs and value. Not everyone is a suitable candidate for corneal refractive surgery, for example, those with very thin corneas, or myopia >-11.00 D, or those with certain corneal diseases, infections or injuries. Most patients who are good candidates will also have good vision with spectacles or contact lenses. Therefore the motivation of going for refractive surgery really depends on how much you want to do away with glasses or contacts, and whether you are willing to pay.
Many people feel it is inconvenient to wear glasses for work, sports or life in general, or that it is ugly to wear glasses, or that it is inconvenient to wear contact lenses. Lots of people become intolerant to contact lenses due to dry eyes, and this is why they elect to have refractive surgery. One should caution if this is the case. As the biggest complication of LASIK or PRK is dry eye, and those intolerant to contact lenses will find dry eye maybe worse after the surgery even if they no longer need to wear contact lenses.
Some people will calculate the expenses of wearing glasses or contact lenses in a life time and compare that to the surgical expenses. Sometimes though, money is not the most decisive factor. It is interesting how humans are. People who don’t need glasses wear plano spectacles to look fashionable, on the other hand, those with -6.00 D myopia struggle all their lives to be glass free. Human eyes are born to be hyperopic and stay slightly hyperopic through millions of years of evolution (except for a very small percentage of people with congenital eye conditions), but modern civilization and education disrupts the natural environment and the way our eyes are meant to be used (well you are reading this article right now). Read more on myopia progression and treatment here and here. Just like obesity, myopia happened, and medicine struggles to correct it.
What is the success rate of LASIK?
We hear a lot of successful stories; sometimes tragic failures. If you are human, you will be affected by the stories around you. However, let’s also take a look at research and statistics. In evaluating almost 60 thousand eyes with LASIK, it has been found that 99.5% of eyes achieve uncorrected vision of 20/40 or better, 90.8% of eyes achieve uncorrected vision of 20/20 or better; 98.6% of eyes reach refraction within 1.00 D of target, and 90.9% of eyes reach within 0.50 D of target refraction; in addition, only 1.2% of all patients are dissatisfied with the outcome [3]. It is not surprising people are paying a lot of money to have this elective surgery. Of course, if your goal is 20/20 vision, there will be a 10% chance that you will not get it. So be prepared.
Is there any risk to refractive surgeries? What are the complications?
In the case of LASIK, it takes about 5 min to complete the procedure in one eye. With topical anesthetic eye drop, it is a painless procedure. The entire process is controlled by computers and rarely does operation mess up.
As mentioned earlier, the most common complication is dry eye, with 20-55% of patients feeling dry, irritated or burning within 6 months of surgery [4]. This is due to injury of corneal nerves during flap incision and laser ablation of the stromal tissue. Some of the nerves will regenerate, but not necessarily recover to the original state. Fortunately most of the dry eye symptoms can be alleviated by regular use of artificial tears.
Other complications are less common, including flap-related problems (flap dislocation, flap wrinkling, ingrowth of epithelium), ocular surface infection and inflammation. These can be corrected by regular follow up visits, or prevented and treated with proper use of antibiotic and/or steroid eye drops.
One rare but dreaded complication is corneal ectasia, which is the bulging and thinning of the cornea after refractive surgery. It happens in only 0.04% to 0.6% of the cases [5], but once it happens, it will be a nightmare for the patient. I once fitted a young woman with rigid contact lens, who had a history of LASIK for -9.00 myopia. She enjoyed 20/20 vision for 1 week, but then everything changed. Corneal ectasia continued progressing, until it finally stabilized at -16.00 myopia with 3 D of irregular astigmatism. Her vision could not be corrected with spectacle lenses or soft contact lenses, and only by wearing rigid contact lenses could she see well for daily functions.
Some of the factors that increase the risk of corneal ectasia post op include [6]:
- The amount of corneal stromal tissue that needs to be removed. The more tissue removed, the more risk for ectasia.
- High myopia- obviously higher the myopia, more tissue needs to be removed, and higher the risk.
- Thickness of the remaining corneal tissue- thinner the remaining tissue, higher the risk.
- Corneal thickness – thin corneas are at higher risk.
- Age- younger patients are more prone to corneal ectasia.
In a nutshell, LASIK cuts away a piece of the corneal tissue, the thicker that tissue is, the higher the risk. In some situations where patients have undiagnosed corneal diseases such as keratoconus, their cornea will progress to thinning and bulging quickly after an insult like LASIK. Therefore it is important to have a complete eye exam pre op, including measuring corneal curvature, thickness and corneal topography, and rule out any corneal diseases.
Recently a technique has been developed to conduct corneal cross-linking in combination with LASIK. Cross-linking is known to increase the mechanical strength of the cornea, and has been used successfully to halt the progression of corneal ectasia in certain corneal diseases such as keratoconus. Among 673 eyes in a study, no corneal ectasia occurred with the combo of LASIK and cross-linking, and less regression found compared to LASIK alone [7]. However, this is currently in clinical research and not used in clinic yet.
Will myopia regress after the surgery?
The stroma of human cornea does not regenerate, once it’s removed, it’s gone forever. This is exactly why LASIK works. However, myopia regression can happen in several situations. 1) The patient is still having myopia progression, that is, their axial length is still growing. This is why LASIK can only be done when prescription is stable. FDA approved LASIK to be done in patients 18 years or older. Even though prescription stabilizes after 18 years of age, it is possible for adults up to 40 years of age to have slow myopia progression if they have prolonged near work. 2) Regression can happen if cornea ectasia occur, and not just frank post-op ectasia, sometimes small amount of corneal changes can happen without being clinically significant or being diagnosed. Those with high myopia or thin corneas may slowly progress another 0.50 or 1.00 D of myopia due to small corneal changes.
Will you be glass free forever after the surgery?
Assume the surgery is successful, free of complications or regression, does that mean you will never need glasses again? The answer is that you may not need glasses to see far away, but you will need reading glasses once you hit presbyopic age (about 40). The current technology only corrects for one refraction per eye- if you choose to see distance clearly, you will need to accommodate to see near. When we get older, our lens becomes more rigid, and won’t be able to change power as we look at near. Maybe in future, LASIK technology allows multiple refractions done on the same eye, then you will not need glasses ever. This is not a dream, as multifocal contact lenses are widely used today and working very well.
Summary
- It is really a personal preference whether to do refractive surgery or not. It is expensive and not covered by insurance.
- If you really want to do it, make sure you go to the eye doctor to have a complete eye exam done and rule out any conditions that contra-indicate refractive surgeries.
- There are a number of corneal refractive surgery techniques, the surgeon will help you choose one that is the most suitable for you based on your eye, your systemic health, your work and your lifestyle.
- 90% people see 20/20, and 98.8% people are happy with the outcome, but you need to know the potential complications, and be informed and prepared.
Do you have any questions, comments or stories to tell? Leave a comment!
References:
- Shen, Z., et al., Dry Eye after Small Incision Lenticule Extraction (SMILE) versus Femtosecond Laser-Assisted in Situ Keratomileusis (FS-LASIK) for Myopia: A Meta-Analysis. PLoS One, 2016. 11(12): p. e0168081.
- Zhang, Y., et al., Clinical Outcomes of SMILE and FS-LASIK Used to Treat Myopia: A Meta-analysis. Journal of Refractive Surgery, 2016. 32(4): p. 256-65.
- Sandoval, H.P., et al., Modern laser in situ keratomileusis outcomes. Journal of Cataract and Refractive Surgery, 2016. 42(8): p. 1224-34.
- Levitt, A.E., et al., Chronic dry eye symptoms after LASIK: parallels and lessons to be learned from other persistent post-operative pain disorders. Mol Pain, 2015. 11: p. 21.
- Randleman, J.B., Evaluating risk factors for ectasia: what is the goal of assessing risk? Journal of Refractive Surgery, 2010. 26(4): p. 236-7.
- Santhiago, M.R., et al., Ectasia risk factors in refractive surgery. Clin Ophthalmol, 2016. 10: p. 713-20.
- Tomita, M., Combined laser in-situ keratomileusis and accelerated corneal cross-linking: an update. Current Opinion in Ophthalmology, 2016. 27(4): p. 304-10.